Resting heart rate variability in regular yoga practitioners – A cross-sectional study
Resting HRV in yoga practitioners
Revised : 2020-06-15
Accepted : 2020-06-16
Online : 2020-06-30
Print : 2020-06-30

Full text
Abstract
Heart rate variability (HRV) is a useful and powerful non-invasive tool for quantitative assessment of cardiac autonomic function. Recent studies have shown that low heart rate variability is an indication of increased risk for cardiac diseases and sudden cardiac death. Yoga has been associated with improved cardio-respiratory performance. Thirty male regular yoga practitioners doing yoga for more than 3 years, age between 25-45 years (yoga group) and 30 male non-yoga practitioners, age-matched (control group) were included. A computerized Niviqure ECG system with HRV software was used for heart rate variability recording. Our results show that frequency-domain parameters like LF power, LF n.u, and LF/HF ratio were significantly lower in yoga group compared to control group. Time-domain parameters like mean RR, NN50, pNN50 were significantly higher in yoga group compared to control group. We conclude that the yoga increases heart rate variability by optimizing the autonomic functions, which is a good indicator of cardiac autonomic activity during rest.
Keywords: Autonomic function, Cardiac diseases, Resting heart rate variability, Yoga
How to cite: Subash S, Sathiyaseelan M, Ramachandran D. Resting heart rate variability in regular yoga practitioners - A cross-sectional study. Ann Med Physiol. 2020 Apr-Jun; 4(2):12-17. doi: 10.23921/amp.2020v4i2.100521
Introduction
Heart rate (HR) is influenced by sympathetic and parasympathetic nervous systems. Heart rate variability (HRV) can be used as a quantitative marker of the autonomic nervous system and is an important index to assess cardiovascular diseases such as hypertension, rhythm disorders, ischemic heart disease, etc [1]. The autonomic nervous system (ANS) is responsible for regulating physiological processes during both healthy and diseased states. The sympathetic system stimulates cardiovascular system (CVS) functioning resulting in increased heart rate, increased stroke volume, systemic vasoconstriction, etc. while the parasympathetic nervous system is charged with the inhibitory tasks of decreasing heart rate, decreasing stroke volume, systemic vasodilatation, etc [2].
HRV is an easy, non-invasive measure for investigating the autonomic influence on the cardiovascular system. HRV describes the variations between consecutive heart beats. These changes from beat to beat occur during physiological responses to various stimuli, including breathing, exercise, mental stress, metabolism, sleep, and even attempt to compensate for the deranged state associated with the disease. The autonomic influence on the cardiovascular system may be evaluated by time-domain and frequency-domain parameters of HRV. A simple method to quantify overall HRV is time-domain analysis, whereas power spectral analysis reveal about different mechanisms responsible for variability in instantaneous heart rate [3]. Decreased HRV can be used as a predictor of congestive heart failure, hypertension, development of diabetic complications and lethal arrhythmic complications [4]. Reduced HRV and baroreflex sensitivity reflect an impaired cardiovagal adaptation, which suggests an overactive sympathetic and/or insufficient parasympathetic drive that is in turn a significant independent predictor of cardiovascular morbidity and mortality. In distinction, high HRV and baroreflex sensitivity are usually considered to be a good indicator of cardiovagal adaptability, with a greater response and sensitivity to changing environmental factors [5].
Yoga is an old system of meditation having psychological, somatic and spiritual components that helps to achieve a harmony between mind, body, and soul. Yoga is commonly perceived and has become a very popular alternative medicine for its minimal expenditure and simplicity. Theoretical explanation of benefits attained by yoga was proposed by Streeter et al [6] wherein yoga reduces the allostatic load in stress response systems such that optimal homeostasis is restored. The reduced drive and GABAergic activity can be corrected by yoga practices resulting in betterment of many disease symptoms. Currently, limited studies are available depicting the resting heart rate variability in the long term and regular practice of yoga. Hence the present study was aimed at investigating resting heart rate variability in regular yoga practitioners compared with non-yoga practitioners.
Materials and methods
This cross-sectional study was conducted after getting approved by an Institutional Ethics Committee at Madras Medical College, Chennai (Approval No. 26082010). The study subjects were recruited based on their willingness and we obtained informed consent from all the subjects. In our study, a total of 60 male subjects were recruited and were divided into two groups.
- Group 1 (Yoga group): 30 male subjects, regular yoga practitioners
- Group 2 (Control group): 30 male subjects, non-yoga practitioners
Inclusion criteria
Group 1: 30 male subjects doing regular yoga for more than 3 years for 30-60 min/day for a minimum of 4 days/week from various yoga centers in Chennai
Group 2: 30 male subjects, non-yoga practitioners were included, Age group between 25-45 years
Exclusion criteria
Females were excluded from the study because of procedural constraints. Individuals with a history of cardiovascular problems, renal disorders, pulmonary function problems, neuromuscular disorders, neurological problems, smoking and alcohol were excluded.
Methodology
After explaining briefly about the study and procedures to the study participants, height (in meters) and weight (in kilograms) was measured and their BMI was calculated. Resting heart rate and blood pressure were measured at rest in a supine position. ECG was recorded using Niviqure (version 53) ECG System (Niviqure Meditech Pvt. Ltd., Bengaluru, India). ECG electrodes are placed and then the subject was made to rest quietly without moving in the awake state with eyes closed, with lights subdued in a supine position for 10-30 minutes. The recordings are performed in a quiet room with controlled room temperature. A continuous ECG recording of 5 minutes (320 sec) at a sampling rate of 1024/sec was done for short term HRV analysis. ECG was acquired from lead II, which contains a maximum peak of the R wave (fiducial point). While acquiring ECG, care was taken to record noise-free, mobile phones switched off, stationary, dysrhythmic events without missing data. After the recording was over the module was then connected to the computer. The analog to digital conversion of the resting ECG signal was done using Analog-Digital (AD) converter with a sampling frequency of 1024/sec. Power spectral analysis of the converted ECG signal was done using Fast Fourier transformation. The data obtained from the selected RR intervals, after removing the violent and arrhythmic artifacts manually, was analyzed through Advanced HRV analysis software version 1.1 (Biomedical Signal Analysis group, University of Kuopio, Finland).
The following precautions were taken while performing the resting HRV
- The subjects were made comfortable.
- Free from stress without any significant anxiety and any recent illness.
- The subjects were tested after 10-30 minutes in a supine position when they were relaxed in resting conditions.
- Compressive garments were removed.
- Subjects were asked to be avoid on the day of testing any beverage containing caffeine, nicotine and alcohol.
- Vigorous exercise was asked to be avoided on the day before testing.
- HRV test was carried out between 10:00 AM – 10:30 AM i. e. 2-2½ hours after breakfast.
- Any other medications that could alter the blood pressure and heart rate were asked to be stopped ideally 24-48 hours before testing.
Parameters studied
Mean HR, Mean RR, NN50, pNN50, LF power, HF power, LF (n.u), HF (n.u), LF/HF ratio.
Time-domain components consisted of mean HR, mean RR, standard deviation of RR intervals (SDNN), square root of the mean of the sum of the squares of differences between adjacent RR intervals (RMSSD), adjacent RR interval differing more than 50 ms (NN50), and NN50 counts divided by all the RR intervals (pNN50).
Frequency-domain components consisted of very low frequency (VLF) component (0.003 to 0.04 Hz), low-frequency (LF) component (0.04 to 0.15 Hz), and high-frequency (HF) component (0.15 to 0.5 Hz) and LF/HF ratio, low frequency power in normalized units (LF nu) = (LF x 100) / (TP–VLF), and similarly HF nu was calculated (HF nu) = (HF x 100) / (TP–VLF). HF, HF nu, SDNN, RMSSD, NN50, and pNN50 reflect cardiovagal tone; LF reflects both the sympathetic and parasympathetic tones; VLF component’s interpretation is not clear, and it cannot be interpreted using short-term HRV recordings; LF nu and HF nu represent a relative tone of the sympathetic and parasympathetic nervous system.
Statistical analysis
All the data obtained was statistically analyzed using SPSS version 17 (SPSS Inc., Chicago, IL, USA). Comparison between the groups were done using independent sample ‘t’ test. The p value of < 0.05 was taken as significant.
Results
In the control group, an increase in the mean heart rate, LF and LF/HF ratio were found. There was a significant decrease in the HF components, which suggested a decrease in the parasympathetic activity and increased sympathetic activity in non – yoga practitioners ( Table 1 ).
| Parameters | Control group | Yoga group | p value |
|---|---|---|---|
| Mean HR | 75.57±9.79 | 67.63±9.36 | 0.002 |
| HF (n.u) | 42.65±7.59 | 57.70±10.74 | 0.000 |
| LF (n.u) | 57.68±7.74 | 42.30±10.74 | 0.000 |
| HF power | 35.06±8.58 | 50.30±10.10 | 0.000 |
| LF power | 47.36±7.75 | 37.06±10.70 | 0.000 |
| LF/HF ratio | 1.44±0.44 | 0.80±0.40 | 0.000 |
| Mean RR | 0.81±0.10 | 1.08±0.37 | 0.000 |
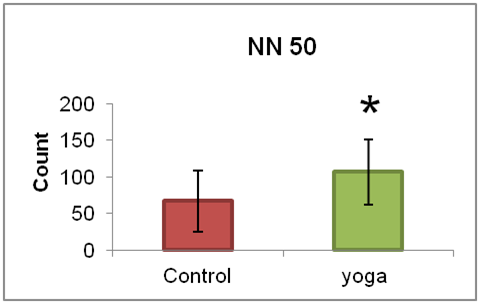
| NN50 | 67.10±41.92 | 106.83±44.63 | 0.001 |
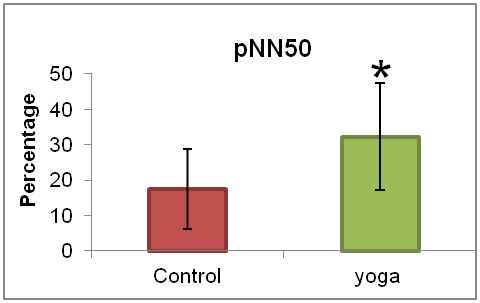
| pNN50 | 17.50±11.25 | 32.20±15.12 | 0.000 |
The HF (n.u), HF power, Mean RR, NN50 and pNN50 were significantly high in the yoga practitioners. This shows the predominance of parasympathetic activity in the yoga group ( Table 1 ).
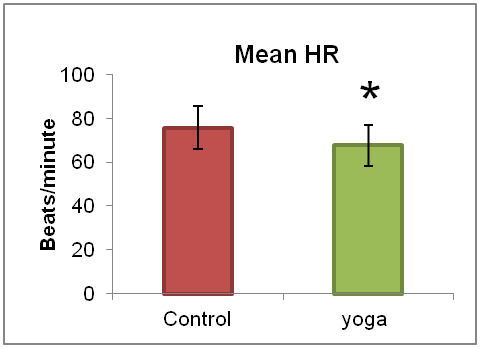
The mean HR was significantly (p=0.002) lower in regular yoga practitioners (67.63±9.36) when compared with non-yoga practitioners (75.57±9.79) ( Figure 1 ).
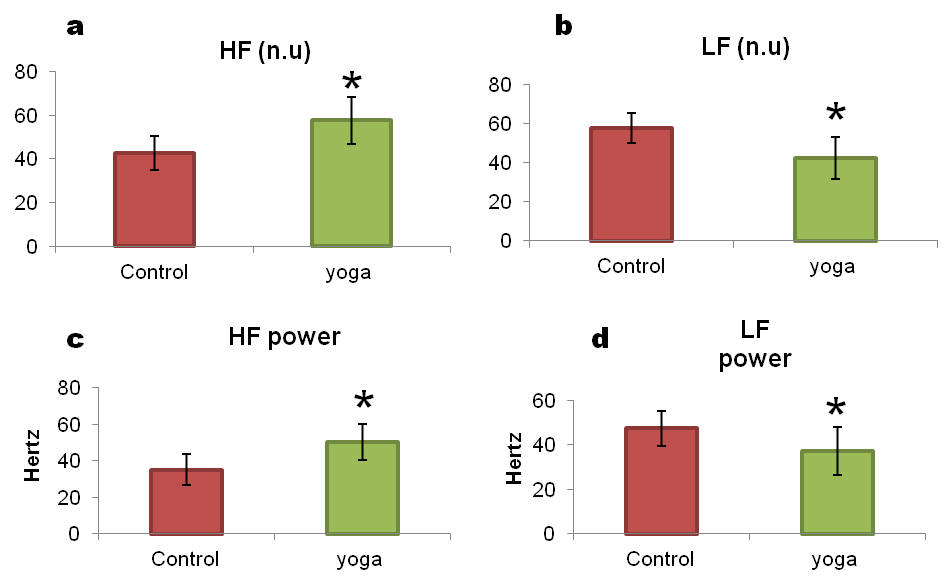
There was a significantly (p=0.000) raised HF (n.u.) in regular yoga practitioners (57.70±10.74) when compared with non-yoga practitioners (42.65±7.59) ( Figure 2a ). The LF (n.u.) was low in yoga group (42.30±10.74) when compared with control group (57.68±7.74) ( Figure 2b ). Similarly, there was a significantly raised HF power in regular yoga practitioners (50.30±10.10) when compared with non-yoga practitioners (35.06±8.58) ( Figure 2c ). Also LF power was significantly lower in yoga group compared to controls ( Table 1 , Figure 2d ).
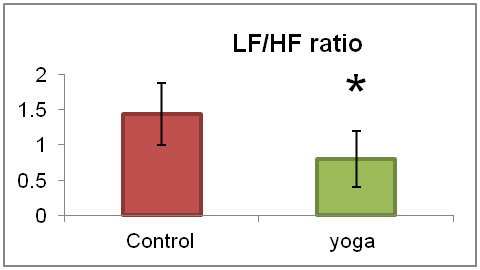
The LF/HF ratio in regular yoga practitioners (0.80±0.40) when compared with non-yoga individuals (1.44 ±0.44) was significantly low (p=0.000) ( Figure 3 ).
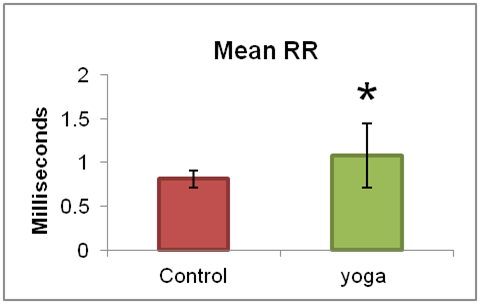
The mean RR interval in regular yoga practitioners (1.08±0.37) when compared with non-yoga practitioners (0.81±0.10) was higher (p=0.000) ( Figure 4 ).
The average NN50 value in yoga group (106.83±44.63) was statistically higher than the control group (67.10±41.92) ( Figure 5 ). Likewise the percentage of pNN50 in regular yoga practitioners (32.20±15.12) when compared with non-yoga practitioners (17.50±11.25) was significantly high ( Figure 6 ).
Discussion
In recent years, as yoga became more popular and yoga classes became more accessible to the public in India, it is important to validate beliefs and confirm claims about yoga’s benefits. Currently, there is a scarcity of well-designed research addressing these specific claims. In the current climate of interest in Complementary and Alternative Medicine (CAM) and Wellness and Health Promotion, it is imperative to address the claims in a manner that does not ignore that yoga is meant to be practiced as a complete system.
There is an extensive literature documenting many determinants of autonomic tone [7]. The stress response is characterized by sympathetic activation, an initial stage which mobilizes the body by either fight-or-flight response, for immediate action. In this stage, the pituitary and hypothalamus sends signals to the sympathetic nervous system.
We come across many internal and external stressors in our daily routine, and if we do not succeed in overcoming it, we may become chronically stressed. Chronic stress leads to negative physical, mental and cognitive impact and also leads to anxiety and depression [8]. Studies show that chronic life stress and diseases are very closely associated [9]. Stress influences the hypothalamus via the limbic system and causes changes in the heart rate variability (HRV) through the autonomic nervous system. HRV may be used to evaluate the mental stress and to determine the status of the autonomic nervous system [10].
In the present study, there was significantly less mean heart rate accompanied with significantly higher mean RR interval in regular yoga practitioners compared with the non-yoga practitioners. This might be due to the calming effects of regular yoga. The practice of yoga provides advantage to many by creating beneficial physiological changes in bodily systems including the nervous system.
Khattab et al reported that relaxation by yoga after 5 weeks of training is associated with a significant increase of cardiac vagal modulation [11]. Another randomized control trial in Brazil reported significant decreases in LF as well as the LF/HF ratio following 4 months of respiratory yoga training [12]. In our study raised HF (n.u.) and HF power was observed in regular yoga practitioners compared with non-yoga practitioners. Also, a significantly lower LF (n.u.) and LF power was observed in regular yoga practitioners compared with non-yoga practitioners.
The LF/HF ratio is considered to emulate sympatho-vagal balance or to reflect sympathetic modulations. In the present study, there was a significantly lower LF/HF ratio in regular yoga practitioners which indicates that sympatho-vagal balance upon regular balance.
In our study there was a significant increase in the NN50 and pNN50 in regular yoga practitioners with a concomitant increase in HF power and HF (n.u.) indicating an increase in the parasympathetic activity after regular yoga training. Yoga practices increases HRV which is an indicator of a healthy autonomic tone.
Conclusion
This study concludes that parasympathetic dominance in regular yoga practitioners as evidenced by decreased heart rate, LF, LF/HF ratio and increased HF power, mean RR, NN50, PNN50. This indicates that there is increased parasympathetic activity and decreased sympathetic activity in regular yoga practitioners. There is increased resting heart rate variability (HRV) in them, which is a good indicator of cardiac autonomic activity during rest and the possibility of reducing cardiovascular disease risks in regular yoga practitioners.
References
- Malik M. Heart rate variability: Standards of measurement, physiological interpretation, and clinical use: Task force of the European Society of Cardiology and the North American Society for Pacing and Electrophysiology. Annals of Noninvasive Electrocardiology. 1996 Apr;1(2):151-181. [Crossref]
- Vanderlei LC, Pastre CM, Hoshi RA, Carvalho TD, Godoy MF. Basic notions of heart rate variability and its clinical applicability. Rev Bras Cir Cardiovasc. 2009 Apr-Jun; 24(2):205-217. [Pubmed] [Crossref]
- Madanmohan, Bhavanani AB, Prakash ES, Kamath MG, Amudhan J. Effect of six weeks of shavasan training on spectral measures of short-term heart rate variability in young healthy volunteers. Indian J Physiol Pharmacol. 2004 Jul; 48(3):370-373. [Pubmed]
- Terathongkum S, Pickler RH. Relationships among heart rate variability, hypertension, and relaxation techniques. J Vasc Nurs. 2004 Sep; 22(3):78-82. [Pubmed] [Crossref]
- Innes KE, Bourguignon C, Taylor AG. Risk indices associated with the insulin resistance syndrome, cardiovascular disease, and possible protection with yoga: a systematic review. J Am Board Fam Pract. 2005 Nov-Dec; 18(6):491-519. [Pubmed] [Crossref]
- Streeter CC, Gerbarg PL, Saper RB, Ciraulo DA, Brown RP. Effects of yoga on the autonomic nervous system, gamma-aminobutyric-acid, and allostasis in epilepsy, depression, and post-traumatic stress disorder. Med Hypotheses. 2012 May; 78(5):571-579. [Pubmed] [Crossref]
- Thayer JF, Lane RD. The role of vagal function in the risk for cardiovascular disease and mortality. Biol Psychol. 2007 Feb; 74(2):224-242. [Pubmed] [Crossref]
- Farah MJ, Noble KG, Hurt H. The developing adolescent brain in socioeconomic context. In: Romer D, Walker EF, editors. Adolescent Psychopathology and the Developing Brain. New York: Oxford University Press; 2007. p.373-387.
- Dimsdale JE. Psychological stress and cardiovascular disease. J Am Coll Cardiol. 2008 Apr 1; 51(13):1237-1246. [Pubmed] [Crossref]
- Appelhans BM, Luecken L. Heart rate variability as an index of regulated emotional responding. Review of General Psychology. 2006 Sep 1; 10(3):229-240. [Crossref]
- Khattab K, Khattab AA, Ortak J, Richardt G, Bonnemeier H. Iyengar yoga increases cardiac parasympathetic nervous modulation among healthy yoga practitioners. Evid Based Complement Alternat Med. 2007 Dec; 4(4):511-517. [Pubmed] [Crossref]
- Santaella DF, Devesa CR, Rojo MR, Amato MB, Drager LF, Casali KR, Montano N, Lorenzi-Filho G. Yoga respiratory training improves respiratory function and cardiac sympathovagal balance in elderly subjects: a randomised controlled trial. BMJ Open. 2011 May 24; 1(1):e000085. [Pubmed] [Crossref]

