Vitamin D status in medical students and risk factor analysis
Vitamin D status in medical students
DOI:
https://doi.org/10.23921/amp.2018v2i1.289803Keywords:
Hypovitaminosis, Immunoassay, Vitamin DAbstract
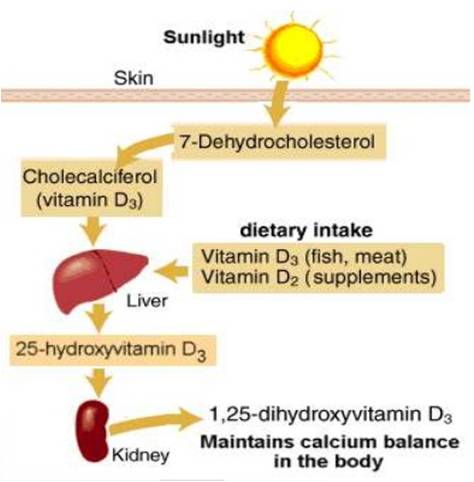
Vitamin D is finding increasing health implications beyond calcium homeostasis. Vitamin D deficiency is prevalent globally including India. Many asymptomatic individuals have hypovitaminosis implicating the need for intervention. The present study aimed at evaluating vitamin D levels among healthy medical students from southern India and its association with well-known risk factors. Hundred apparently healthy medical students between the age group of 18-25 years were recruited based on defined inclusion and exclusion criteria. A questionnaire form with details of sun exposure, tanning, milk intake, general health and drug history were obtained. Vitamin D levels were assessed by chemiluminescent immunoassay (CLIA). Vitamin D values were considered normal for 30-60 ng/ml, deficient for <20 ng/ml and insufficient for levels between 21-29 ng/ml. Majority of the students (89%) had deficient 25-hydroxyvitamin D levels while 8% of the student had insufficient and 3% of the students had sufficient 25-hydroxyvitamin D levels. The mean 25-hydroxyvitamin D level was 14.01±6.20 ng/ml, median level was 12.95 ng/ml and ranged between 5.15 to 43.01 ng/ml. No statistically significant association was noted with sex, BMI, sun exposure, dietary intake or serum calcium levels. To conclude, vitamin D deficiency is highly prevalent in asymptomatic medical students and showed lack of relationship with the well-defined risk factors in literature prompting to look for newer risk factors in this country.
Downloads
Metrics
References
Pfotenhauer KM, Shubrook JH. Vitamin D deficiency, its role in health and disease, and current supplementation recommendations. J Am Osteopath Assoc. 2017 May 1; 117(5):301-5.
Bouillon R, Carmeliet G, Verlinden L, van Etten E, Verstuyf A, Luderer HF, Lieben L, Mathieu C, Demay M. Vitamin D and human health: lessons from vitamin D receptor null mice. Endocr Rev. 2008 Oct; 29(6):726-76.
Prentice A. Vitamin D deficiency: a global perspective. Nutr Rev. 2008 Oct; 66(10 Suppl 2):S153-64.
Bolek-Berquist J, Elliott ME, Gangnon RE, Gemar D, Engelke J, Lawrence SJ, Hansen KE. Use of a questionnaire to assess vitamin D status in young adults. Public Health Nutr. 2009 Feb; 12(2):236-43.
Wacker M, Holick MF. Sunlight and vitamin D: A global perspective for health. Dermatoendocrinol. 2013 Jan 1; 5(1): 51-108.
Pike JW, Christakos S. Biology and mechanisms of action of the vitamin D hormone. Endocrinol Metab Clin North Am. 2017 Dec; 46(4):815-43.
van Schoor N, Lips P. Global overview of vitamin D status. Endocrinol Metab Clin North Am. 2017 Dec; 46(4):845-70.
Forrest KY, Stuhldreher WL. Prevalence and correlates of vitamin D deficiency in US adults. Nutr Res. 2011 Jan; 31(1):48-54.
Arneson WL, Arneson DL. Current methods for routine clinical laboratory testing of vitamin D levels. Lab Med. 2013 Feb 1; 44(1):e38-e42.
WHO Scientific Group on the Prevention and Management of Osteoporosis (2000: Geneva, Switzerland). Prevention and management of osteoporosis: report of a WHO scientific group. WHO Tech Rep Ser. 2003; 921:1-164. Available from http://www.who.int/iris/handle/10665/42841 (Last accessed February 17, 2018)
Bouillon R, van Schoor NM, Gielen E, Boonen S, Mathieu C, Vanderschueren D, Lips P. Optimal vitamin D status: a critical analysis on the basis of evidence-based medicine. J Clin Endocrinol Metab. 2013 Aug; 98(8):E1283-304.
Man RE, Li LJ, Cheng CY, Wong TY, Lamoureux E, Sabanayagam C. Prevalence and determinants of suboptimal vitamin D levels in a multiethnic Asian population. Nutrients. 2017 Mar 22, 9(3):E313.
Babu US, Calvo MS. Modern India and the vitamin D dilemma: evidence for the need of a national food fortification program. Mol Nutr Food Res. 2010 Aug; 54(8):1134-47.
Selvarajan S, Gunaseelan V, Anandabaskar N, Xavier AS, Srinivasamurthy S, Kamalanathan SK, Sahoo JP. Systematic review on vitamin D level in apparently healthy Indian population and analysis of its associated factors. Indian J Endocrinol Metab. 2017 Sep-Oct; 21(5):765-75.
Sowah D, Fan X, Dennett L, Hagtvedt R, Straube S. Vitamin D levels and deficiency with different occupations: a systematic review. BMC Public Health. 2017 Jun 22; 17(1):519.
Zabihiyeganeh M, Jahed SA, Sarami S, Nojomi M. Hypovitaminosis D: are medical students at risk? Int J Prev Med. 2014 Sep; 5(9): 1161-8.
Published
How to Cite
Issue
Section
License
Copyright (c) 2018 Quench Academy of Medical Education and Research (QAMER)

This work is licensed under a Creative Commons Attribution 4.0 International License.
The authors warrants and represents that the submitted MANUSCRIPT is an original work and has not been published before in any form, and that it does not infringe upon any copyright or other right(s), that it does not contain infringing, libelous, obscene or other unlawful matter, that he/she is the sole and exclusive owner of the rights here-in conveyed to the Publisher, and that he/she has obtained the customary permission from the copyright owner or his legal representative whenever a text/passage from copyrighted material is quoted or a table or illustration from such material is used. The Author(s) will indemnify the Publisher for, and hold the Publisher harmless from any loss, expense or damage occasioned by any claim or suit by a third party for copyright infringement or arising out of any breach of the foregoing warranties as a result of publication of the Article. The Article shall be delivered to the Publisher free of copyright charges. In the event that the Article is not accepted and published by Publisher, this agreement becomes null and void.
Sherpa/Romeo publisher policy can be viewed at Annals of Medical Physiology - Sherpa/Romeo Policy
Plum X metrics
Article level metrics are shown here